Proteomic Analyses of Clots Identify Stroke Etiologies in Patients Undergoing Endovascular TherapyKim, Jung, Kim
et alCNS Neurosci Ther (2025) 31 (3), e70340
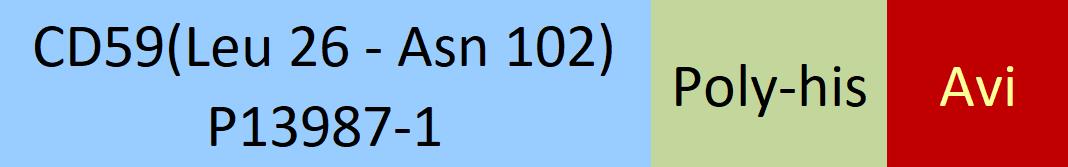
Abstract: This study aimed to investigate the correlation between clot composition and stroke mechanisms in patients undergoing endovascular therapy (EVT), using proteomic analysis.This study included 35 patients with ischemic stroke (cardioembolism [CE], n = 17; large artery atherosclerosis [LAA], n = 6; cancer-related [CR], n = 4; and undetermined (UD) cause, n = 8) who underwent EVT. Retrieved clots were proteomically analyzed to identify differentially expressed proteins associated with the three stroke mechanisms and to develop the machine learning model.In the discover stage, 3838 proteins were identified using clot samples from 27 patients with CE, LAA, and CR mechanisms. Through functional enrichment and network analysis, 149 proteins were identified as potential candidates for verification studies. After verification experiments, 34 proteins were selected as the final candidates to predict stroke mechanisms. Furthermore, the machine learning-based model identified three proteins associated with each mechanism (Pleckstrin in CE; CD59 glycoprotein in LAA; and Immunoglobulin Heavy Constant Gamma 1 in CR) in the UD group.This study identified specific protein markers of clots that could differentiate stroke mechanisms in patients undergoing EVT. Therefore, our results could offer valuable insights into elucidating the mechanisms of ischemic stroke, which could provide information on more effective secondary prevention strategies.© 2025 The Author(s). CNS Neuroscience & Therapeutics published by John Wiley & Sons Ltd.
Claudin-2 enhances human antibody-mediated complement-dependent cytotoxicity of porcine endothelial cells by modulating antibody binding and complement activationLi, Yang, Yang
et alFront Immunol (2025) 16, 1547512
Abstract: Immune rejection represents a significant barrier to transplantation, especially in the context of xenotransplantation. Endothelial cells (ECs) derived from pigs serve as the initial barrier against the human immune system in xenotransplantation. Tight junction proteins are essential components of endothelial cell tight junctions; however, their role in xenotransplantation has been less thoroughly investigated. Claudin-2, a key tight junction protein, was investigated here for its role in human antibody-mediated complement-dependent cytotoxicity (CDC).Using an in vitro model of human antibody-mediated CDC, we assessed the effect of Claudin-2 on porcine aortic endothelial cells (PAECs) and porcine iliac endothelial cells (PIECs). Claudin-2 expression was either knocked down or overexpressed in these cells. A flow cytometry assay was used to evaluate C3c, C9, and the C5b-9 deposition, as well as the extent of human IgM and IgG binding to PIECs. The mRNA levels of complement regulators (CD46, CD55, CD59, Factor H, Factor I) were quantified by real-time PCR.The loss of Claudin-2 protected PAECs and PIECs from human antibody-mediated CDC, while the overexpression of Claudin-2 enhanced the cytotoxicity in PAECs and PIECs within the same model. Unexpectedly, the loss or overexpression of Claudin-2 did not influence the mRNA expression levels of complement regulators (CD46, CD55, CD59, Factor H, and Factor I). Importantly, the loss of Claudin-2 significantly decreased the deposition of the C5b-9 complex, commonly referred to as the membrane attack complex (MAC), whereas the overexpression of Claudin-2 enhanced the deposition of the C5b-9 complex, indicating that Claudin-2 facilitates complement activation. Furthermore, the loss of Claudin-2 resulted in a decrease in the deposition of C3c and C9 on PIECs. Moreover, Claudin-2 enhanced human antibody binding to porcine ECs, as evidenced by increased IgG and IgM binding.Our findings indicate that Claudin-2 enhances the cytotoxicity of porcine ECs through modulating antibody binding and complement activation. The deficient of Claudin-2 in genetically modified pigs is likely to protect porcine ECs and enhance xenograft survival in pig-to-human organ or tissue xenotransplantation.Copyright © 2025 Li, Yang, Yang, Song, Xu, Wu, Li, Chen, Chen, Yu, Xie, Yang, Zhou, Luan and Gao.
Urine complement analysis implies complement activation is involved in membranous nephropathyXu, Li, Zhang
et alFront Med (Lausanne) (2025) 12, 1515928
Abstract: The onset and progression of membranous nephropathy (MN) have been associated with complement activation, yet the overall characteristics of this activation in the kidneys remain unclear. In our study, we utilized urine proteomic data to investigate the features of complement activation. We examined the relationship between urine complement components and both clinicopathological features and clinical outcomes in patients with MN.Differential expression proteins (DEPs) analysis was performed using proteomic data from urine samples collected from 50 patients with MN, 50 patients with IgA nephropathies (IgAN), and 72 healthy controls (HC). Then, Gene Ontology and Kyoto Encyclopedia of Genes and Genomes analyses were carried out on the DEPs identified in MN. We further investigated the differentially expressed urinary complement proteins in MN patients, exploring their relationships with clinicopathological features and clinical remission. Next, 11 representative complements were selected for validation. Immunohistochemistry and immunofluorescence techniques were employed to compare the expression of CD59 and C5b-9 in renal tissues from MN patients, with analyses conducted on both the clinical remission group and the no remission group (n = 6 in each group).Total 1,427 differentially expressed proteins were identified between the MN and HC groups. KEGG pathway analysis showed significant enrichment of these DEPs in the complement-activated pathway within the MN group. Additionally, a correlation was found between proteinuria and the levels of 27 urinary complement proteins. Notably, Collectin12 (collec12) and C1s were positively correlated with tubular atrophy/interstitial fibrosis (TIF) and monocyte infiltration. Furthermore, urine CD59 emerged as a predictor of clinical remission. Lower deposition of C5b-9 in renal tissue and higher expression of CD59 were detected in clinical remission group than non-remission group.In patients with MN, abnormal levels of complement components in urine are commonly observed. Currently, the use of complement inhibitors has brought new hope for the treatment of MN. The factor B inhibitor LNP023 and the factor D inhibitor BCX9930 are undergoing clinical trials for the treatment of MN. Our study indicates that complement abnormalities could serve as clinical biomarkers for tracking the progression of MN, predicting clinical remission, and guiding targeted complement therapy for those affected.Copyright © 2025 Xu, Li, Zhang and Li.
Identification and Validation of a Novel Prognostic Signature of Gastric Cancer Based on Seven Complement System-Related Genes: An Integrated AnalysisZhang, Zhu, Yang
et alCrit Rev Eukaryot Gene Expr (2025) 35 (3), 1-22
Abstract: The complement system (CS) is linked to the progression of gastric cancer (GC), which has a high mortality rate, though its mechanisms in GC remain unclear. This study aims to identify CS-related prognostic genes with causal links to GC, and to investigate their mechanisms. The intersection between differentially expressed genes (DEGs) obtained from the TCGA-STAD dataset and CS-related genes (CRGs) was defined as differentially expressed CRGs (DCRGs). Prognostic genes with a causal association with GC (pCDCRGs) were sequentially identified via Mendelian randomization (MR) analysis and Cox and least absolute shrinkage and selection operator (LASSO) regression analyses, followed by expression analysis. A gene signature and a nomogram were then established based on pCDCRGs and independent prognostic factors. Subsequent analyses focused on functional enrichment, immune relevance, drug sensitivity, gene interactions, and molecular regulatory networks. Eventually, reverse transcription-quantitative PCR (RT-qPCR) was employed to validate expression of pCDCRGs. DCRGs were obtained from the intersection of 8,418 DEGs and 241 CRGs. Among 12 DCRGs with causal association (CDCRGs) with GC, 7 genes were identified as pCDCRGs, including FANCG, FANCF, F2R, C4BPA, SERPINF2, PROC, and CD59. Notably, CD59 was markedly highly expressed in the normal group, whereas the other genes were markedly highly expressed in the GC group. Afterward, an accurate pCDCRG signature was developed. Risk score, age, and stage were recognized as independent risk factors, and the constructed nomogram demonstrated strong predictive accuracy. Additionally, analyses indicated that these 7 pCDCRGs may influence GC by affecting pathways such as complement and coagulation cascades, immune cell infiltration, immune characteristics, immunotherapy responses, and drug sensitivity. These effects may be linked to gene interactions and the regulatory roles of lncRNAs like RMRP and miRNAs such as hsa-mir-613. RT-qPCR showed C4BPA, PROC, F2R, and SERPINF2 were markedly up-regulated, whereas CD59 was markedly down-regulated in GC tissues. This study identified seven complement system-related prognostic genes with causal links to GC, based on which we developed a highly predictive 7-pCDCRG signature, providing valuable insights for clinical prognostic prediction and immunotherapy in GC patients.























































 膜杰作
膜杰作 Star Staining
Star Staining

















